Connect with us
Published
3 years agoon

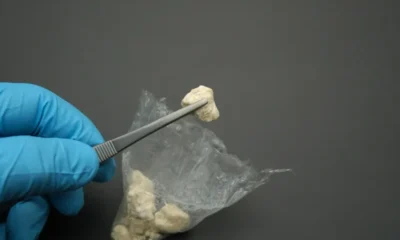
As many countries around the world are seeing the benefits of cannabis research and legislation opening up, especially to help treat medical conditions, we not only witness the amazing benefits of the plant, but also the detriment to individuals when they do not have access to the help and treatments they need.
Recently, a family in Edinburgh, Scotland had the latter experience. Karen Gray’s eight-year-old son Murray would have hundreds of seizures a day before he started to take the cannabis-based drug Bedrolite, which they bought from the Netherlands. The drug costs £1,300 a month, or around $1,800. When Murray’s brother, 13-year-old Dean, wrote to First Minister Nicola Sturgeon, urging the politician to help make medications like this more affordable for people like his brother, they were disheartened by the response.
Sturgeon said that she was “deeply sorry” to read about the difficulties Murray faces and that, while she has “enormous sympathy” for the circumstances, she indicated that the medication has to be proven safe before it will be available on the NHS, Scotland’s publicly funded healthcare system.
“In order to prescribe medicines like those Murray currently takes on the NHS in Scotland, we need stronger evidence of their safety than we currently have,” Sturgeon’s letter reads. “Just now, specialist doctors in the NHS who treat children with epilepsy and similar medical conditions aren’t confident enough about prescribing cannabis oils, including Bedrolite, until there is better evidence available following a clinical trial.”
Sturgeon says they have recently been in touch with the company that supplies young patients in the UK with cannabis oils, encouraging them to take part in future clinical trials, and that they are working with other governments around the UK to develop the medicines and build evidence. She ends the letter saying she asked the Chief Pharmaceutical Officer to explore what more they could do to help the family, before thanking Dean for the letter.
Karen said the letter was disappointing and didn’t help her son, telling BBC News, “We are delighted and grateful that the first minister took the time to write to us—it did seem like a very personal letter. But it’s infuriating because she is saying about safety and the NHS won’t prescribe the medicine, but the NHS is prescribing the very same cannabis oil to two other children in the UK.”
Murray’s seizures are brought on by severe, complex epilepsy called Doose Syndrome, and his anti-epilepsy medicine has caused him serious side effects. Karen said that Murray was basically dying in the hospital and the NHS couldn’t do anything for him.
“The only way to take the cannabis oil legally was to get a private neurologist,” she said. “She writes the prescription because she knows it’s safe for Murray. He hasn’t had a seizure in two years and no side-effects.”
Only three medical cannabis products have been licensed by the UK-wide medicines and Healthcare products Regulatory Agency since legalization in 2018. These include Taivex, used to treat severe spasticity in MS patients, Nabilone, for chemotherapy-induced nausea and Epidyolex, for rare forms of childhood epilepsy; only Epidyolex can be prescribed by the NHS in Scotland.
The family tried this medication for Murray, who initially responded, though Karen reported it stopped working, she believes because it did not contain tetrahydrocannabinol (THC).
And while Sturgeon argues that the NHS needs to go through the procedures to ensure the medicine’s safety, Bedtrolite has already changed Murray’s life dramatically.
“Now, he is able to go to school full-time, he runs about. He is having no seizures and no side-effects, when he was having loads of side-effects with all the anti-epileptic drugs that he was given,” Karen said. “It’s just infuriating that there are children in the UK being prescribed the exact same cannabis oil that Murray takes through the NHS. It’s just not fair at all.”
Currently the family raises the funds to pay for the cost of the monthly prescription with the help of friends and family, though she fears there will come a time when they can no longer afford the prescription. Karen said she planned to reply to the first minister to further explain the situation.
Peter Carroll, director of the End Our Pain campaign lobbying for financial help for families like Karen’s paying thousands of pounds on private prescriptions, echoed Karen’s sentiments, saying the response was touching but that the letter from the first minister didn’t address the point.
“Families like Karen’s have proved beyond doubt that the medication is life-transforming. If the issue is safety, then Karen has the best evidence it is safe,” Carroll said. “Our appeal is that now is the time to cut across the bureaucracy and give these families some money to pay for private prescriptions while they work on more widespread prescribing.”


German Authorities to Ban Cannabis Smoking, Vaping at Festivals Including Oktoberfest


Ohio Company Signs Deal To Grow Hemp for Bioplastic


Gen Z Consumes Less Alcohol, Prefers More Cannabis and Non-Alcoholic Beverages


Colorado Senate Approves Legislation Banning Social Media Praise of Drugs

Study: CBD for Crack Use Disorder Comparable to Traditional Treatments, Less Side Effects


Snoop Dogg’s Dr. Bombay Ice Cream Launches New Flavor for 4/20
