Connect with us
Published
11 months agoon

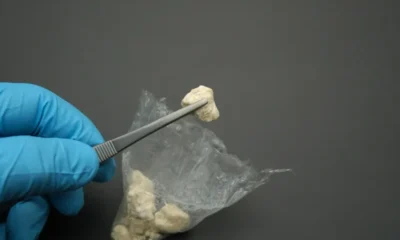
New Zealand has allowed for the broad use of medical cannabis since December 2018, when the Misuse of Drugs Act was amended. Now, new research is providing insight on how patients perceive the effects of medical cannabis, pointing to its positive effects on a number of symptoms.
The study, titled “Patients experiences of therapeutic cannabis consumption in New Zealand,” was published in the journal Drugs, Habits and Social Policy. Of the 213 people in the study who used cannabis medicinally, nearly 96% reported that it helped with a number of conditions. Additionally, 49% said they were able to reduce or entirely stop taking prescription medications due to their medicinal cannabis use.
According to the abstract, the purpose of the study was to explore the experiences of medical cannabis patients, aiming to gather real-word evidence about the products patients use and the positive and negative effects they experienced.
Researchers from the University of Otago, Victoria University and the University of Auckland collaborated on the study. It was designed as an exploratory study, utilizing a survey and semi-structured interviews. The findings focus on thematic analysis of five of the open-ended survey questions, while interview data were not reported on.
Specifically, 95.6% of participants said that cannabis was beneficial. The most common three themes across the thematic analysis showed that cannabis assisted with pain relief, sleep and anxiety. In regard to pain management, 96% of participants said cannabis was helpful; 97% said cannabis helped with sleep, and 98% said it helped with mental health issues. Among participants who took cannabis for other reasons, like autism, ADHD, post-traumatic stress disorder and difficulty eating, 98% said cannabis was beneficial.
Participants also reported negative effects, though they were relatively minor and experienced by 28% of participants. Some participants also referenced that negative effects were due to sourcing cannabis from the illicit market.
According to study co-author Dr. Geoff Noller, from the Dunedin School of Medicine’s Bioethics Centre, the study results are consistent with several others conducted in Aotearoa New Zealand and internationally, specifically in regard to the positive effects cannabis has on pain relief, sleeplessness and insomnia, Medical Xpress reports.
Noller also highlighted the amount of participants who were able to decrease or stop the use of prescription drugs, many opioid based, because of their medicinal cannabis use.
“This both reinforces that they experienced some actual effect from using cannabis in that they ceased or decreased other medications with recognized efficacy, and in the case of many of these other medications, they reduced their use of potentially more problematic medications,” Noller said. “Opioids, for example, have well known issues in terms of dependence and other negative side effects.”
That said, Noller and the other researchers said this doesn’t suggest that prescription medication shouldn’t be used or that people should use one or the other. Noller said that “there is a place for both approaches,” though this study’s results point to the potential for cannabis to treat specific symptoms and conditions, especially those “refractory to treatment by conventional means.”
Ultimately, Noller indicated that this relies on an affordable, widely accessible medical cannabis program. Nodding to a previous study he was involved in, Noller referenced that the majority of people using cannabis therapeutically sourced it through the illicit market. Noller said that the current regulations “appear to be creating problems for many New Zealanders” who report positive benefits from medicinal cannabis, according to Medical Xpress.
Specific barriers include cost—specifically that products on the market today are too expensive for many residents due to “compliance costs of production imposed by regulations — along with the lack of knowledge among physicians, which Noller said results in a reluctance to prescribe in many instances.
Noller said these results point to the need to reevaluate the current policies, especially those that create barriers to medicinal cannabis access. Part of that is embracing more real-world cannabis studies, he said, and going more creative clinical research to highlight the efficacy of medicinal cannabis.
“But this takes funding and commitment from researchers who may feel nervous about working with cannabis, with its history of illicit use due to historic policies that are now being reformed,” Noller said. “These attitudes need to change.”


German Authorities to Ban Cannabis Smoking, Vaping at Festivals Including Oktoberfest


Ohio Company Signs Deal To Grow Hemp for Bioplastic


Gen Z Consumes Less Alcohol, Prefers More Cannabis and Non-Alcoholic Beverages


Colorado Senate Approves Legislation Banning Social Media Praise of Drugs

Study: CBD for Crack Use Disorder Comparable to Traditional Treatments, Less Side Effects


Snoop Dogg’s Dr. Bombay Ice Cream Launches New Flavor for 4/20
