Connect with us
Published
3 years agoon

It’s undeniable that cannabis research increasingly shows how using the plant and derivative products can be beneficial for treating pain and a number of conditions. However, three new studies presented at the 2021 Annual Meeting of the American Academy of Orthopaedic Surgeons (AAOS) show cannabis use before total knee arthroplasty (TKA) and total hip arthroplasty (THA) can lead to increased complications, longer stays in the hospital, higher rates of adverse events, more readmissions and higher costs.
The studies will work to inform future research and will help orthopaedic surgeons to educate and work with patients prior to surgery. An arthroplasty is the surgical reconstruction or full replacement of a joint, and many folks in need of these types of surgeries will find they need some relief in pain management, leading to the increase in cannabis as an alternative option.
The medical and recreational boom of cannabis is undeniable, both boasting a major increase in usage, including an increase among older populations. A recent study in the Journal of the American Medical Association showed that cannabis use among older adults (65 and above) in the US has steadily increased over time, specifically observing an increase in use from 2.4 percent to 4.2 percent from 2015 to 2018.
However, this data—although clearly displaying the influx in use among older Americans—leaves questions surrounding the outcomes of surgeries like TKA and THA that, up until now, have little to no research in regard to their relationship with cannabis as a pre-surgical treatment for pain relief.
AAOS researchers used a large insurance database to retrospectively review 3,308 TKA patients between 2010 and 2018 to assess both 90-day and one-year outcomes (including opioid consumption, readmissions, surgical revisions and complications) with matching cohorts of patients who consumed cannabis pre-op versus those who didn’t.
The results noted that dislocation rates were significantly higher among cannabis users over nonusers at both 90 days and one year; opioid consumption and revision rates were similar, or at least not significantly different, between both groups at 90 days, and revisions and complications were similar in occurrence at 90 days and one year.
In addition, investigators studied how cannabis use disorder (CUD), or the pattern of using progressively larger amounts of cannabis over a period of time, interacts with outcomes following primary TKA. They used a private database of 55,553 patients enrolled in the CUD and case-matched populations to perform a retrospective look over January 1, 2008 to March 21, 2018.
This study found that CUD patients had a significantly longer hospital stay compared to their counterparts (3.61 versus 2.07 days), and from 2010 to 2018, the average for CUD patients increased from 2.93 days to 3.93 days. CUD patients also had a significantly higher likelihood (28.08 percent versus 12.5 percent) of developing medical complications within 90 days, including but not limited to pneumonia, respiratory failures, myocardial infarctions, cerebrovascular accidents and acute kidney injuries.
Additionally, CUD was associated with higher rates of prostheses-related complications compared to the control group (9.63 percent versus 5.16 percent), and patients with CUD had significantly higher day-of surgery costs ($24,292.15 versus $20,616.40) and total, global 90-day episode of care costs ($29,025.34 versus $24,258.17).
A third study aimed to look at the same CUD patients undergoing a THA surgery, looking at a private database of 44,154 patients who underwent primary THA from January 1, 2008 to December 31, 2018.
Researchers found very similar results in their study of THA patients with CUD versus the TKA patients with CUD: CUD patients undergoing primary ThA also had significantly longer hospital stays compared to the control group (four versus three days), CUD patients experienced a higher frequency of adverse events (11.23 percent versus 4.82 percent, ii.e. higher rates of pneumonia, respiratory failure, cerebrovascular accidents, urinary tract infections and acute renal failure) and CUD patients had a higher total global 90-day care cost ($24,585.96 versus $23724.93).
While some of this information appears daunting, especially for folks looking to treat their pain without turning to opioids, it is a sign that the research to follow will only continue to inform orthopaedic surgeons and the practice as a whole in regard to preoperative treatment and cannabis use.


Congressional Progressive Caucus Says Dems Can Legalize MJ By Winning House, Senate Majorities This November


Cannabis Industry Has 440,000 Full-Time Workers
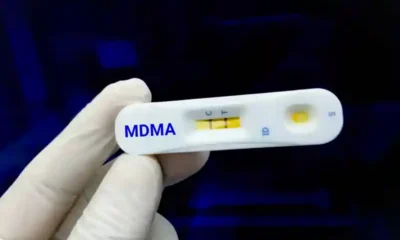

Federal Register Proposes Adding Fentanyl, Removing MDMA From Drug Testing Panels


Feds File Charges Against Maine Weed Grower After Probe Spanning 20 States


The Cannabis Market Is Booming in Japan


German Authorities to Ban Cannabis Smoking, Vaping at Festivals Including Oktoberfest
